 SATURDAY, March 9 (HealthDay News) -- Women with advanced ovarian cancerwho receive intense chemotherapy directly into their stomach area may live at least one year longer than women who receive standard intravenous chemotherapy, a new study says.
SATURDAY, March 9 (HealthDay News) -- Women with advanced ovarian cancerwho receive intense chemotherapy directly into their stomach area may live at least one year longer than women who receive standard intravenous chemotherapy, a new study says.
But this survival edge may come at the expense of more side effects.
"The long-term benefits are pretty significant," said study author Dr. Devansu Tewari, director of gynecologic oncology at the Southern California Permanente Medical Group, in Orange County. "There is no study of ovarian cancer treatmentsthat has shown a greater survival advantage."
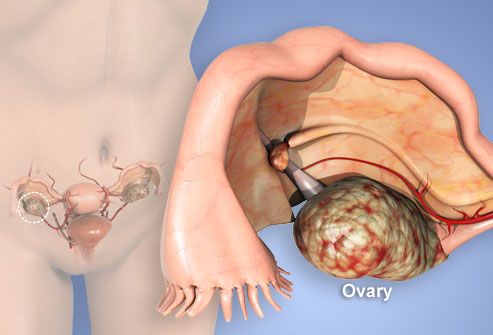
Intraperitoneal chemotherapy involves bathing the abdominal area with chemotherapy agents. By contrast, intravenous (IV) chemotherapy is delivered throughout the body via the bloodstream. The U.S. National Cancer Institute currently recommends intraperitoneal therapy for women with ovarian cancer who have had successful surgery to remove the tumor.
The 10-year follow-up data from two studies of nearly 900 women with advanced ovarian cancer will be presented Saturday at the annual meeting of the Society of Gynecologic Oncology, in Los Angeles.
In 2013, more than 22,000 American women will be diagnosed with ovarian cancer, and more than 14,000 will die from the disease, according to the U.S. National Cancer Institute. There are no early screening tests for ovarian cancer, which is why it is often diagnosed when the cancer has already spread outside of the ovaries. For this reason, survival rates tend to be very low.
In the new study, women who received the intraperitoneal treatment were 17 percent more likely to survive longer than those who got IV chemotherapy. On average, women in the intraperitoneal group survived for more than five years, while those who received IV chemotherapy survived for about four years, the study found.
 But survival benefits aside, intraperitoneal chemotherapy does confer a greater risk of side effects -- such as abdominal pain and numbness in the hands and feet -- and not all women can tolerate this high concentration of cancer-killing drugs. The drugs are also absorbed more slowly, providing more exposure to the medicine. The same properties that make the intraperitoneal therapy more effective likely play a role in causing more side effects, the researchers said.
But survival benefits aside, intraperitoneal chemotherapy does confer a greater risk of side effects -- such as abdominal pain and numbness in the hands and feet -- and not all women can tolerate this high concentration of cancer-killing drugs. The drugs are also absorbed more slowly, providing more exposure to the medicine. The same properties that make the intraperitoneal therapy more effective likely play a role in causing more side effects, the researchers said.
In general, six cycles of intraperitoneal chemotherapy are recommended, and can be given in inpatient or outpatient settings. The more cycles the women completed, the greater their survival advantage, the study showed. After five years, close to 60 percent of women who completed five or six cycles of intraperitoneal therapy were still alive, compared with 33 percent of those who completed three or four cycles and 18 percent of those who completed one or two cycles. Women can switch back to IV chemotherapy if the side effects prove too harsh. Still, the researchers said, some intraperitoneal chemotherapy is better than no
Younger and healthier women were among the most likely to complete the regimen.
"If after surgery all of the visible cancer has been removed and there is no cancer that is greater than 1 centimeter left in any one area, a woman is an immediate candidate [for intraperitoneal chemotherapy]," Tewari said. "If someone is older and in good shape and handled the operation well, they are also candidates."
Growing numbers of doctors and women with ovarian cancer are opting for intraperitoneal therapy, she said. And it may offer even greater benefits when paired with some of the newer therapies for ovarian cancer that are moving through the drug development pipeline.
"Its use can and should increase," said Tewari, who also is an assistant professor of obstetrics and gynecology at the University of California, Irvine, School of Medicine.
Dr. Jubilee Brown, a spokeswoman for the Society of Gynecologic Oncology and an associate professor of gynecologic oncology at the University of Texas MD Anderson Cancer Center, said the new findings are exciting.
"This is long-term follow-up data that confirms what we expected," Brown said. "We have been waiting for years to determine if the results are short-lived or if we see it years later, and now we know that we see the survival benefit 10 years out."
"Doctors are used to giving IV chemotherapy, so this is a new skill set in terms of giving the drugs," she said. "It comes with different equipment and patient instructions and side effects. As individual physicians and centers become more comfortable and confident with learning how to manage the side effects, its use will increase."
Dr. Elizabeth Poynor, a gynecologic oncologist at New York City's Lenox Hill Hospital, agreed. "The toxicity and intensity is greater than with IV therapy, so some people can't tolerate it," she said. "But for those who do, survival is clearly benefited."
"It's a tradeoff," Poynor said. "There are more side effects, but there are also survival benefits. You don't know how you will tolerate it until you try -- and if it's not for you, you can back off."
Because this study was presented at a medical meeting, the data and conclusions should be viewed as preliminary until published in a peer-reviewed journal.